- First Touch
- Posts
- Breast Cancer Awareness Month: A Few Things To Know About Mammograms, Screenings, and Practical Ways to Lower Your Risk💕🎀🌸💘
Breast Cancer Awareness Month: A Few Things To Know About Mammograms, Screenings, and Practical Ways to Lower Your Risk💕🎀🌸💘
I wanted to find a way to create a deeper connection with my followers and provide more insights into the content I share on other platforms. I'm excited to give you all a closer, more personal look into my world—sharing insights from my life, my research, and work.
Breast Cancer Awareness Month
Every year during Breast Cancer Awareness Month, the conversation around early detection takes center stage — reminders to schedule mammograms, check for lumps, and stay proactive about screenings are everywhere. While detection matters, it’s equally important to understand what influences breast health in the first place. I wanted to share a few key things to know about breast cancer screening and prevention. 🎀
A few things to consider about mammograms:
Mammograms have long been the gold standard screening tool for breast cancer. They work by using X-rays to create images of the breast tissue, helping to detect abnormalities, including tumors, at an early stage.
The goal is early detection: identifying cancers before they spread. Standard recommendations suggest women begin regular mammograms in midlife (around age 40).
While mammograms are beneficial in certain cases, there are also some significant downsides that deserve attention. It’s important to understand their limitations. No screening tool is perfect. Every patient should understand the drawbacks, the benefits, and the concerns.
Benefits:
Early detection: Mammograms are effective at identifying breast cancer early, often before a lump can be felt. This is important because early-stage breast cancer is more treatable and has a higher survival rate.
Widely available: Mammograms are a standard screening method and are easily accessible in most healthcare systems. They are often covered by insurance and recommended annually or biennially for women over 40 or with a family history of breast cancer.
Effective for detecting calcifications: Mammograms are particularly useful for spotting calcifications—small calcium deposits in the breast that may indicate the presence of early-stage breast cancer or precancerous conditions.
Drawbacks
Radiation exposure: Mammograms expose women to ionizing radiation, which can actually increase the risk of tissue damage and cancers. There is a concern about cumulative exposure over many years, especially because breast tissue is highly sensitive.
False positives: Mammograms can lead to false positives, where an abnormality is detected but turns out to be benign. This can result in unnecessary stress, additional tests, and biopsies, which carry their own risks and emotional toll.
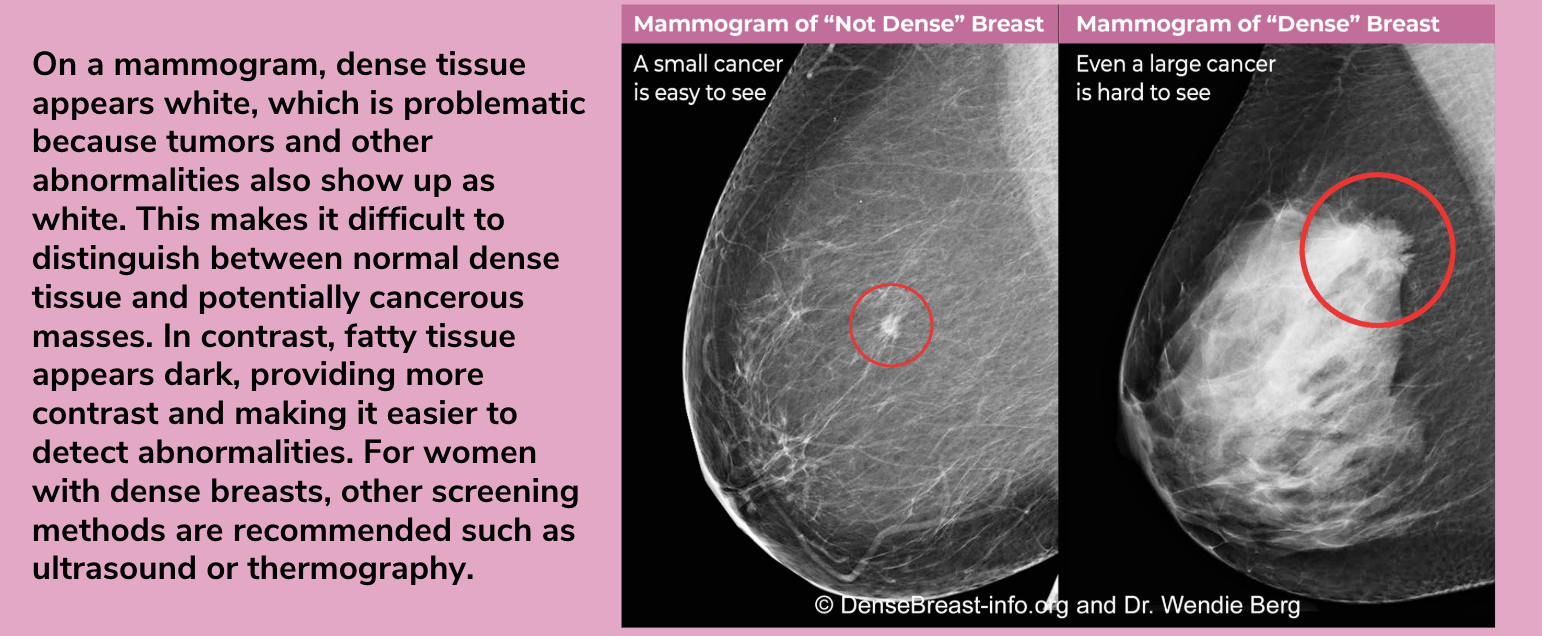
Less effective for dense breasts: Women with dense breast tissue often experience less accurate mammograms because dense tissue and tumors both appear white on the X-ray, making it harder to detect cancer.
Pain and discomfort: The compression of breast tissue required during a mammogram and necessary to get a clear image, but can be painful or uncomfortable for many women.
Concerns
Overdiagnosis: One of the more concerning aspects of mammograms is overdiagnosis—when a mammogram detects cancers that are slow-growing and may never cause harm during a woman’s lifetime. These "indolent" cancers may lead to unnecessary treatments, including surgery, chemotherapy, or radiation, which have significant side effects.
Limited benefit for younger women: Mammograms are less effective in younger women (under 40) due to denser breast tissue. For this group, mammograms might not be as beneficial, and the risk of false positives is higher.
Missed cancers (false negatives): In some cases, mammograms can miss cancers, particularly in women with dense breast tissue or those with fast-growing tumors. A false negative can create a false sense of security, delaying diagnosis and treatment.
Mammograms have become the standard of care in breast cancer screening, and most doctors are expected to recommend them as part of routine health checks for women. In fact, a doctor who advises against a mammogram could be seen as deviating from established medical guidelines, raising concerns about liability or non-compliance with standard practice.
One of the most significant issues with mammograms, however, is overdiagnosis. Since it’s not possible to know whether a cancer will be harmful or not, all are treated as dangerous. This leads to unnecessary interventions such as chemotherapy, radiation, or disfiguring surgeries, which can harm otherwise healthy women.
A common contributor to overdiagnosis is carcinoma in situ, which refers to abnormal cell changes that are not technically cancer. Studies have shown that many cases of carcinoma in situ never develop into invasive cancer, yet they are often treated as if they were, leading to overtreatment.
A study published in the Annals of Internal Medicine found that after 10 years of annual mammograms, studies show that 50-60% of women will likely experience at least one false positive result.
False positives often lead to additional diagnostic procedures, such as more imaging tests, follow-up mammograms, or biopsies. For example, it’s estimated that 28,000 unnecessary needle biopsies are performed each year as a result of screening, and there has been a sharp increase in mastectomies, particularly for carcinoma in situ, even though many of these cases would never have progressed to invasive cancer.
It’s also estimated that 20% of breast cancers are missed by mammograms. This number increases to 50% if you have dense breasts. Dense breasts refer to breasts that have a higher proportion of fibrous and glandular tissue compared to fatty tissue. This is a normal variation and can be found in many women, particularly those who are younger, though density can persist in older women as well. Breast density is usually determined through a mammogram, but it’s not something that can be felt during a physical exam.
Some experts suggest that mammograms have taken on a near "religious" status, with an unwavering belief in their benefits, despite substantial evidence showing the risks. Mammograms are often promoted as life-saving tools that protect women from breast cancer, but research suggests that these benefits are overstated, and the harm from overdiagnosis is significant.
We’ve reached a point where mammograms are almost seen as mandatory for every woman, every year, without question. However, avoiding conversations about the potential downsides of mammograms does women a disservice. Every woman is different, with her own unique physiology and risk factors, and she may need a personalized screening plan. Blind adherence to annual mammograms for every woman may not be the best approach, and encouraging more open, informed discussions around the true impact of these screenings can help ensure that we make the most appropriate choices for our health.
Other screening options:
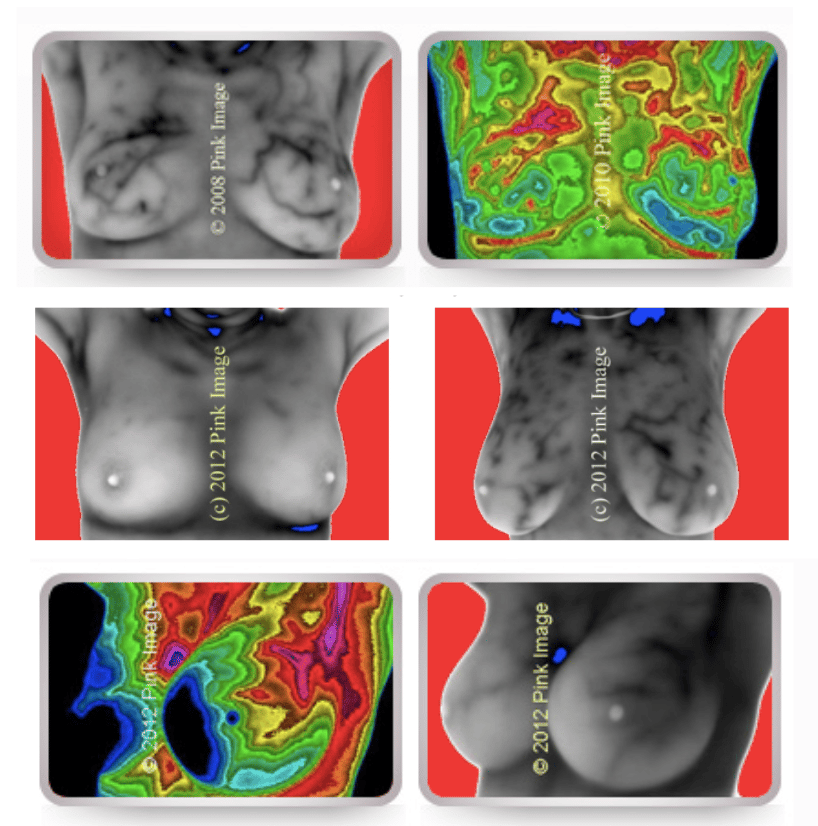
Thermograms use infrared technology to detect heat patterns and changes in blood flow within the breast. Increased vascularity can signal inflammation or abnormal tissue growth, such as the formation of new blood vessels that support a tumor's nutrient supply.
Pros:
Non-invasive and radiation-free.
Comfortable. Since there’s no compression involved, it’s a pain-free option.
Capable of detecting inflammation, which can indicate early-stage changes before a tumor forms.
Cons:
Does not provide a clear picture of the breast.
Small, deep-seated tumors may not cause enough temperature variation to be detected.
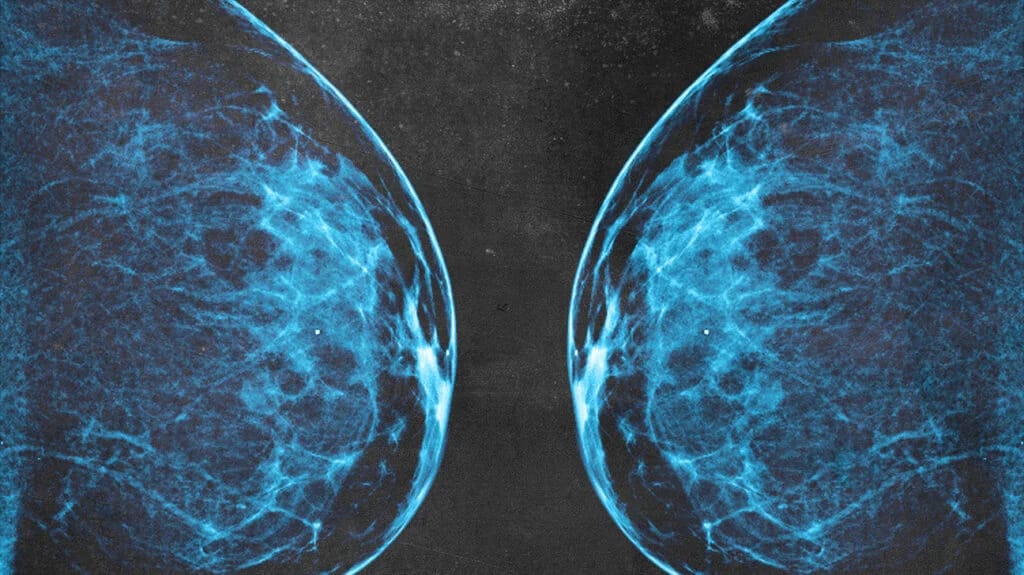
Quantitative Transmission (QT) Breast Imaging uses transmission ultrasound to create 3D images of the breast by sending sound waves through the breast tissue.
Pros:
Radiation-free and non-invasive.
Effective for dense breast tissue.
Comfortable. Since there’s no compression involved, it’s a pain-free option.
Provides a clear, high resolution picture of the breast.
Can detect breast calcifications.
Requires less time than a traditional ultrasound.
Cons:
Limited availability.
Limited insurance coverage.
In 2017, the FDA approved QT Imaging, and we are now offering scans at the center. This is a new technology that we are excited to to make more available! It provides one of the clearest pictures of the breast health.
To schedule a QT scan or thermogram, you can visit here or call us at 949-680-1880 to book your appointment!

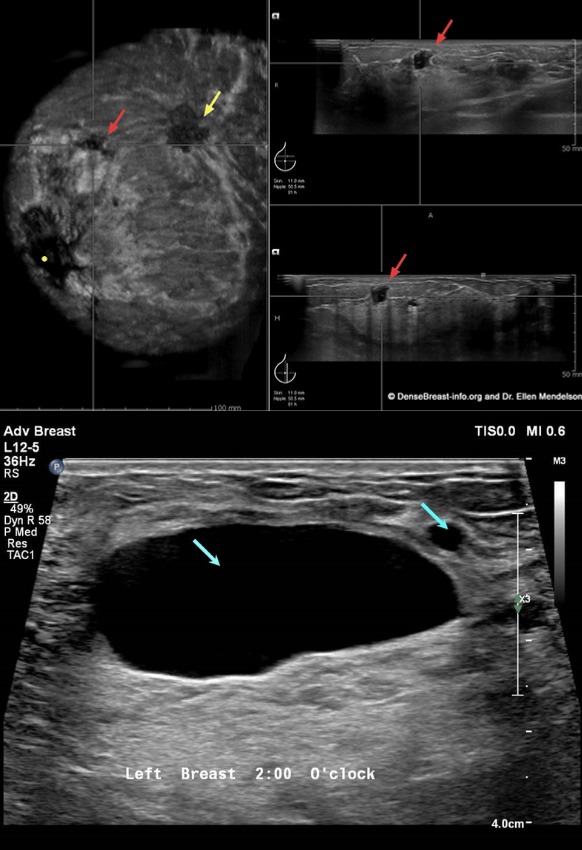
Hand-Held Ultrasound (HHUS) devices use sound waves to capture real-time images of the breast, particularly useful for identifying lumps or abnormalities.
Pros:
Radiation-free and non-invasive.
Effective for dense breast tissue.
Comfortable. Since there’s no compression involved, it’s a pain-free option.
Provides a real-time picture of the breast.
Cons:
Operator-dependent. Accuracy of the results can depend on the skill of the technician performing the ultrasound.
Takes more time than other screening methods.
Can only detect calcifications if they are large.
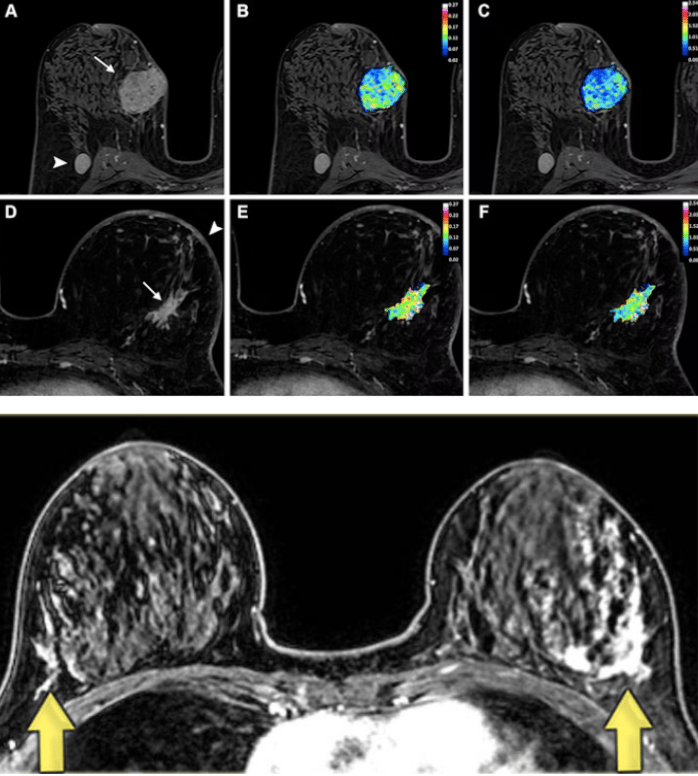
Breast Magnetic Resonance Imaging (MRI) uses powerful magnetic fields and radio waves to generate detailed, cross-sectional images of the breast.
Pros:
Radiation-free.
Effective for dense breasts.
Comfortable. Since there’s no compression involved, it’s a pain-free option.
Provides clearest pictures of the breast.
Can detect breast calcifications.
Cons:
May require a gadolinium-based contrast injection into a vein in the arm.
This contrast dye helps highlight breast tissue during MRI scans, but small amounts of gadolinium can remain in the body, accumulating in the brain and bones over time, especially with repeated imaging. It’s best to ask whether contrast is truly necessary or if a non-contrast MRI can provide similar information.Takes more time than other screening methods.
Can be expensive.
Can produce false positives.
No screening method is perfect, so I think it is important that women understand the nuances of each option. Sometimes multiple methods are needed to get the full picture of a woman’s breast health.
If you’re seeking support with early detection, have recently received a breast cancer diagnosis, or want to explore integrative options for prevention and treatment, please contact us.
A few practical things you can do to lower your risk of breast cancer:
While screening plays an important role, if we truly want to help women, the real key is prevention. We need to understand the many factors that contribute to breast cancer—then actively reduce exposure to them—while also supporting the conditions that keep breast tissue healthy and resilient.
Less than 4% of the National Cancer Institute’s budget goes toward cancer prevention research. Meanwhile, little attention is given to the well-documented, avoidable drivers of disease such as excess estrogen, radiation exposure, and chemical pollutants.
There should be just as much focus on preventing cancer as there is on detecting it. Women deserve more than reactive care. Finding cancer early is valuable, but helping the body stay well in the first place is far more powerful.
Prevention requires a whole-body, whole-lifestyle approach. Here are a few things I personally do:
Make sure my estrogen and progesterone levels are balanced. The health of the breast depends on the ratio of estrogen to progesterone. Progesterone is anti-cancer, anti-proliferation, anti-inflammatory, pro-differentiation. Progesterone is highly protective against breast cancer. Estrogen on the other hand, stimulates cellular proliferation, promotes growth, increases inflammation and contribute to DNA damage. When elevated and unopposed by progesterone, it can contribute to breast cancer. Unfortunately, progesterone declines rapidly under stress stress and as we age, leaving breast tissue more vulnerable to unopposed estrogen. In some cases, supplementation is necessary to restore balance. My favorite option is Raena, which provides bioidentical progesterone at physiologic levels levels the body naturally produces)without fillers, chemicals, or dyes. They also have at-home hormone tests to determine your estrogen to progesterone ratio.
Limit exposure to endocrine-disrupting chemicals. Avoid plastics, synthetic fragrances, conventional cleaning products, and cosmetics with parabens or phthalates. Araza is great for makeup (code: CONNEALY15) , Branch Basics for cleaning products (CODE: CONNEALYMD) .
Get sunlight and support vitamin D levels. Vitamin D is needed for the synthesis of progesterone and helps regulate cell growth.
Ensure adequate intake of nutrients like niacinamide, iodine, magnesium, vitamin A, vitamin E, and calcium to promote healthy progesterone levels.
Support thyroid health. The thyroid sets the pace for every cell in the body, including the breast. Low thyroid function slows metabolism, reduces progesterone, and allows estrogen to become dominant, all conditions that can promote breast tissue growth and increase cancer risk. The thyroid needs adequate protein, selenium-rich foods, natural light exposure, and stress management to keep hormones in healthy rhythm.
Minimize unnecessary synthetic hormone use. Long-term use of hormonal birth control or synthetic hormone replacement therapy should be discussed carefully, especially if cancer risk is a concern.
Support liver detoxification. The liver breaks down estrogen. Support it with B vitamins, adequate protein and carbohydrates. Sauna, filtering water, drinking coffee, and using nontoxic cookware can all help reduce the toxic burden on the liver. I like liver protect and calcium D glucarate to promote healthy liver function and reduce estrogen levels. Regular season liver flushes, castor oil packs, and detox baths are also helpful.
Prioritize restorative sleep. Poor sleep disrupts circadian rhythm, raises cortisol, and throws off hormone balance, especially progesterone.
Take care of my nervous system, spend time with loved ones, and practice gratitude and affirmations. Chronic stress elevates cortisol, suppresses thyroid and progesterone levels, and increases inflammation, all of which can make breast tissue more vulnerable. Practices that calm the nervous system, like time in nature, connection with loved ones, and daily affirmations of gratitude, help shift the body into a parasympathetic, healing state.
Apply topical iodine on the breast. Iodine is essential for the health of breast, thyroid, and reproductive tissues. The breasts naturally concentrate iodine, which helps regulate normal cell growth, balance estrogen’s effects, and maintain soft, healthy tissue. Low iodine levels are linked to fibrocystic breast changes and may contribute to the development of fibroids and other estrogen-dominant conditions. Topical iodine, when used appropriately, supports these tissues by promoting differentiation (cells maturing normally) and reducing excessive proliferation and the risk of breast cancer.
Use aspirin as an anti-inflammatory (when needed): Aspirin can reduce chronic inflammation and inhibit excess estrogen signaling, both of which are associated with a lower risk of hormone-related cancers.
The second edition of The Cancer Revolution is here!
In honor of Breast Cancer Awareness Month, I’m excited to share that the updated edition of The Cancer Revolution is now available. While this book explores all types of cancer, it’s especially relevant for women seeking to understand how to prevent, detect, and treat breast cancer in a more comprehensive and integrative way.
This edition has been fully revised with the latest research on hormone balance, metabolism, nutrition, toxins, and early detection—key areas that directly influence breast health. You’ll also find new sections on how to strengthen the immune system, support the body during treatment, and create an internal environment that’s resistant to disease.
Whether you’re focused on prevention, navigating a current diagnosis, or supporting recovery, this book is designed to help you know what to do, what to ask, and how to make informed, empowering decisions about your care.
My hope is that it gives women clarity and confidence—that it helps you feel equipped, not afraid. Because when you understand what drives disease, you also understand how to heal. 💕

Talk soon ❤️,
Dr. C